- Home
- ASHRM
- Advancing Health Care Risk Management
- CPHRM
- CPHRM - Certified Professional in Health Care Risk Management (CPHRM)
ASHRM CPHRM Certified Professional in Health Care Risk Management (CPHRM) Exam Practice Test
Certified Professional in Health Care Risk Management (CPHRM) Questions and Answers
Which of the following concepts is integral to supporting a Safety Culture in a healthcare organization?
Options:
disciplining an employee
trending occurrences
assigning blame
speaking up
Answer:
DExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, a culture of safety is grounded in open communication, transparency, and shared accountability. An essential element of safety culture is the expectation that all staff members feel empowered and psychologically safe to speak up about concerns, near misses, unsafe conditions, or potential errors without fear of retaliation.
Speaking up supports early identification of risks and fosters continuous improvement. It aligns with just culture principles, which distinguish between human error, at-risk behavior, and reckless conduct, promoting learning rather than automatic punishment. Encouraging staff to voice concerns strengthens teamwork, situational awareness, and patient-centered care.
While trending occurrences is an important analytical tool for quality improvement, it is a process measure rather than a core cultural principle. Disciplining employees and assigning blame, when applied indiscriminately, undermine trust and discourage reporting, thereby weakening safety culture.
Clinical and patient safety objectives emphasize communication, accountability, and nonpunitive reporting environments. Therefore, speaking up is integral to supporting and sustaining a safety culture within a healthcare organization.
What is one advantage of avoluntaryerror reporting system over amandatoryerror reporting system?
Options:
Voluntary systems guarantee legal privilege in all states
Voluntary systems typically elicit more frontline reports and near-misses
Voluntary systems eliminate the need for root cause analysis
Voluntary systems replace peer review and credentialing
Answer:
BExplanation:
Voluntary reporting systems often generatemore reports, especially ofnear-misses and low-harm events, because staff perceive less punitive risk and greater learning value. This is crucial for proactive risk management: near-misses expose weak signals and system vulnerabilities before a patient is harmed. A robust voluntary culture supports a “just culture” approach—encouraging reporting while still holding people accountable for reckless behavior. Compared with mandatory systems (typically limited to defined serious events), voluntary systems improve the organization’s ability to identify patterns (communication failures, workflow traps, labeling issues, staffing risks), prioritize interventions, and measure improvement over time. Risk management objectives include earlier hazard detection, better trend analysis, and stronger safety culture. To maximize effectiveness, leadership must provide feedback loops (“you reported, we improved”), protect confidentiality where permitted, and couple reporting with structured analysis (RCA/FMEA). While voluntary reporting does not automatically confer legal privilege, it is a foundational learning system in high-reliability healthcare operations.
An emergency department physician has evaluated and stabilized a patient who needs a sign language interpreter. The on-call physician is consulted for admission. Which of the following regulatory laws are most relevant?
Options:
ADA and EMTALA/COBRA
HCQIA and ADA
EMTALA/COBRA and HIPAA
HIPAA and HCQIA
Answer:
AExplanation:
Under Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, two federal laws are most directly implicated in this scenario: the Americans with Disabilities Act ADA and the Emergency Medical Treatment and Labor Act EMTALA, formerly enacted under COBRA.
EMTALA requires hospitals with emergency departments to provide an appropriate medical screening examination, stabilization of emergency medical conditions, and appropriate transfer or admission regardless of ability to pay. Since the emergency physician has evaluated and stabilized the patient and the on-call physician is being consulted for admission, EMTALA obligations remain central to ensuring compliant continuation of care.
The ADA is also directly relevant because it mandates that health care organizations provide reasonable accommodations to individuals with disabilities, including effective communication. For a patient requiring a sign language interpreter, the hospital must provide appropriate auxiliary aids and services to ensure meaningful access to care.
HIPAA relates primarily to privacy and protected health information, while HCQIA addresses peer review immunity and credentialing matters. Therefore, ADA and EMTALA are the most relevant regulatory frameworks in this case.
A hold-harmless agreement is an important component of which of the following aspects of a risk financing program?
Options:
risk transfer
risk retention
first-party liability insurance
third-party liability insurance
Answer:
AExplanation:
Within Health Care Risk Management frameworks established by ASHRM and the American Hospital Association Certification Center, risk financing strategies include risk retention, risk transfer, and insurance mechanisms. A hold-harmless agreement is a contractual provision in which one party agrees to assume responsibility for certain liabilities and to protect another party from claims or losses arising from specified activities. This mechanism is a classic example of risk transfer.
Through hold-harmless or indemnification clauses, an organization shifts potential financial responsibility for loss to another party, often a contractor, vendor, or service provider. This contractual allocation of liability reduces the organization’s exposure without necessarily purchasing insurance. It is therefore categorized under noninsurance risk transfer.
Risk retention, by contrast, involves assuming and financing losses internally, such as through self-insurance or deductibles. First-party liability insurance addresses losses sustained directly by the insured organization, while third-party liability insurance covers claims made by others against the organization. Although insurance is also a method of risk transfer, the specific instrument described in the question is a contractual transfer mechanism rather than an insurance product.
Accordingly, a hold-harmless agreement is most directly associated with risk transfer within a comprehensive risk financing program.
Which of the following is a program of the Food and Drug Administration FDA post market surveillance system for medical devices that requires healthcare facilities to report patient deaths or injuries related to a medical device?
Options:
Safe Medical Devices Act SMDA
Emergency Medical Treatment and Active Labor Act EMTALA
Occupational Safety and Health Act of 1970 OSHA
Patient Safety Organization PSO
Answer:
AExplanation:
Under Health Care Risk Management standards recognized by ASHRM and the American Hospital Association Certification Center, the Safe Medical Devices Act SMDA is part of the FDA’s post market surveillance system for medical devices. The SMDA requires healthcare facilities to report to the FDA and, in some cases, to the manufacturer when a medical device has or may have caused or contributed to a patient death or serious injury. This mandatory reporting system enhances device safety monitoring and supports regulatory oversight after products enter the market.
EMTALA governs emergency medical screening and stabilization obligations, not device reporting. The Occupational Safety and Health Act focuses on workplace safety for employees rather than patient device-related injuries. Patient Safety Organizations operate under the Patient Safety and Quality Improvement Act and facilitate voluntary reporting of patient safety events, but they do not replace FDA-mandated device reporting requirements.
Legal and regulatory objectives in healthcare risk management emphasize compliance with federal reporting statutes, timely submission of required reports, and maintenance of documentation to mitigate regulatory exposure. Therefore, the Safe Medical Devices Act is the correct answer regarding mandatory FDA post market surveillance reporting for device-related deaths or injuries.
For a risk management program to be effective, it needs:
Options:
Organizational commitment, visibility/access, and physician engagement
Only a policy manual
Only insurance coverage
Only incident reporting software
Answer:
AExplanation:
Effective risk management requires more than tools—it needs organizational commitment (tone at the top), operational visibility (access to events, leaders, data), and physician engagement because many high-severity risks involve medical decision-making and clinical leadership. Risk management objectives include preventing harm (patient safety), reducing financial loss (claims and insurance costs), ensuring compliance, and building a learning culture. Without executive and board support, corrective actions stall; without visibility, emerging risks are missed; without physician buy-in, clinical process redesign fails. Successful programs integrate with quality, patient safety, compliance, legal, and operations, and they use structured methods (RCA/FMEA, audits, claims trend analysis) to drive measurable improvement. This also strengthens defensibility: it shows governance, action, and continuous improvement—key elements in regulatory review and litigation.
Which of the following factors should be considered when setting or adjusting indemnity reserves?
incurred medical expenses
emotional pain and suffering
medical expert witness costs
future cost of medical care
Options:
1, 2, and 3 only
1, 2, and 4 only
1, 3, and 4 only
2, 3, and 4 only
Answer:
BExplanation:
According to Health Care Risk Management principles established by ASHRM and the American Hospital Association Certification Center, indemnity reserves represent the estimated amount the organization expects to pay in settlement or judgment to a claimant. Indemnity refers specifically to damages paid to compensate the injured party, not defense or administrative expenses.
Incurred medical expenses are a core component of economic damages and must be included in indemnity reserve calculations. Emotional pain and suffering fall under non-economic damages and are also considered when estimating potential settlement or verdict value. Future cost of medical care is another essential factor, particularly in cases involving long-term injury or disability, as it represents projected economic damages that may substantially increase exposure.
Medical expert witness costs, however, are categorized as defense expenses and are typically included in allocated loss adjustment expenses rather than indemnity reserves. These costs relate to the defense of the claim rather than compensation to the plaintiff.
Risk management objectives emphasize accurate differentiation between indemnity and expense reserves to ensure proper financial reporting and regulatory compliance. Therefore, incurred medical expenses, pain and suffering, and future medical costs should be considered when setting indemnity reserves, while expert witness costs should not.
In preparing next year's budget, the hospital CFO has contacted the risk manager for a projected contribution to the hospital's professional and general liability self-insured retention fund. To respond to this request, the risk manager should refer to which of the following?
Options:
actuarial reports and loss runs
professional and general liability premiums
frequency and severity analyses of pending claims
total incurred losses for the current year
Answer:
AExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, projecting contributions to a self-insured retention fund requires actuarially sound financial forecasting. Actuarial reports use historical claims data, trend analyses, loss development factors, and exposure projections to estimate future liabilities and required funding levels. Loss run reports provide detailed historical claims information, including paid losses, reserves, and claim status, which serve as foundational data for actuarial modeling.
Professional and general liability premiums are relevant to insured layers above the retention but do not determine funding requirements for the retained portion. Frequency and severity analyses of pending claims are important components of actuarial evaluation but, standing alone, may not capture long-tail development or incurred but not reported claims. Total incurred losses for the current year provide limited insight without considering historical patterns and future projections.
Risk financing objectives emphasize accurate funding of retained risk to ensure financial stability, regulatory compliance, and protection of organizational assets. Therefore, actuarial reports, supported by comprehensive loss run data, provide the most reliable basis for determining projected contributions to a self-insured retention fund.
Generally, an incident is defined as:
Options:
Any happening not consistent with routine care/operations (including near-misses)
Only events that cause death
Only patient complaints
Only billing disputes
Answer:
AExplanation:
Broad incident definitions (including near-misses and unsafe conditions) support proactive risk management. If reporting is limited only to severe harm, the organization loses learning opportunities from early warning signals. Risk management objectives favor capturing deviations from expected process—falls without injury, specimen labeling near-misses, medication dispensing discrepancies—because these events reveal system vulnerabilities that can later cause major harm. Strong incident management includes classification, timely review, escalation thresholds, root cause analysis for significant events, and feedback to frontline staff. This approach aligns with systems-based safety: identify hazards, implement controls, and monitor effectiveness.
If a practitioner requests a telemedicine consult with another practitioner in another state, the consultant:
Options:
May need to hold a valid license in the patient’s state (requirements vary by state)
Never needs any license
Can practice under the patient’s insurance plan only
Can rely on verbal permission from the ED nurse
Answer:
AExplanation:
Telemedicine licensure is largely state-based in the U.S., and many states require the consulting clinician to be licensed in the state where the patient is located (with exceptions such as specific compacts, special telehealth registrations, or emergency provisions). Risk management objectives include verifying licensure/credentialing before services, ensuring privileging-by-proxy processes where applicable, confirming malpractice coverage for telehealth and cross-state practice, and ensuring informed consent/privacy safeguards. Failure to comply can trigger regulatory penalties, payer issues, and liability exposure if care is delivered without proper authorization.
Which of the following wouldnotbe considered an emergency condition for EMTALA purposes (as a general example set)?
Options:
Myocardial infarction
Ruptured appendix
Active labor with complications
Stable chronic kidney failure without acute destabilization
Answer:
DExplanation:
EMTALA applies when an individual comes to the ED and requires a medical screening exam to determine whether anemergency medical condition (EMC)exists. Conditions like myocardial infarction, ruptured appendix, and unstable labor can constitute EMCs because absence of immediate medical attention could reasonably be expected to place health in serious jeopardy. By contrast,stable chronic kidney failurewithout acute destabilization may not meet the EMC threshold—though the screening exam must be performed before that determination is made. Risk management objectives emphasize: never “triage out” without an appropriate screening exam, document findings and decision-making, and apply consistent policies to avoid discriminatory practice. EMTALA failures often stem from process breakdowns (delays, refusal, inadequate screening, improper transfer), so standardized ED workflows and training are critical.
A risk manager is reviewing the professional liability insurance policy for the limits of liability. Which of the following should the risk manager review FIRST?
Options:
conditions
exclusions
declaration
insuring agreement
Answer:
CExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, the declarations page is the first section a risk manager should review when assessing limits of liability in a professional liability insurance policy. The declarations page summarizes key policy information, including named insureds, policy period, coverage types, limits of liability per occurrence and aggregate, deductibles or self-insured retentions, endorsements, and premium details.
Because the question focuses specifically on limits of liability, the declarations page provides the most direct and concise statement of coverage limits. It serves as the policy’s summary and reference point for determining financial exposure and coverage structure.
The insuring agreement defines the scope of coverage and triggers for defense and indemnity obligations but does not list specific limit amounts. Exclusions outline what is not covered, and conditions specify policyholder responsibilities such as notice and cooperation requirements. While all sections are important for comprehensive review, the declarations page is the appropriate starting point when verifying coverage limits.
Risk financing objectives emphasize careful policy analysis to ensure alignment between coverage limits and organizational risk exposure. Therefore, the declarations page should be reviewed first when assessing limits of liability.
An original contract could contain:
Options:
Effective date, insurance requirements, and contract terms
Only a logo and slogan
Only verbal promises
Only a price estimate without scope
Answer:
AExplanation:
Healthcare contracting is a risk control tool. Core terms include effective date, scope, responsibilities, performance standards, indemnification, andinsurance requirements(limits, additional insured, notice of cancellation). Clear terms reduce disputes, clarify liability allocation, and strengthen compliance (HIPAA BAAs, data security, subcontractor controls). Risk management objectives focus on preventing uninsured exposures and ensuring vendors meet safety, credentialing, and regulatory requirements—especially for clinical services, technology, and facility operations.
An appropriate way to complete the verification read-back of a complete order, as required by The Joint Commission National Patient Safety Goals, is to have the person receiving the order
Options:
write the information down before reading it back.
immediately repeat the information.
have a witness verify that the information is repeated back correctly.
document the date and time the order was received.
Answer:
AExplanation:
According to Health Care Risk Management standards supported by ASHRM and The Joint Commission National Patient Safety Goals, the read-back process is designed to ensure accurate communication of verbal or telephone orders. The correct process requires the person receiving the order to first write down the complete order and then read it back to the prescribing practitioner for verification.
Writing the order down before reading it back reduces reliance on memory and decreases the risk of omission or transcription errors. The practitioner who gave the order must then confirm that the read-back is accurate. This closed-loop communication process enhances patient safety and reduces medication and treatment errors associated with miscommunication.
Immediately repeating the information without documenting it does not meet the full verification requirement, as the written record must be confirmed. A witness is not required under the standard. Documenting the date and time is necessary for proper charting but does not constitute completion of the read-back verification itself.
Clinical and patient safety objectives emphasize clear, structured communication processes. Therefore, writing the information down before reading it back is the appropriate method to complete the verification process.
What is responsible for many HIPAA privacy violations in practice?
Options:
Impermissible access/disclosure (including “snooping” without a job-related need)
Correctly authorized disclosures
Proper encryption practices
De-identification
Answer:
AExplanation:
A frequent HIPAA Privacy Rule violation isimpermissible access or disclosureof protected health information—commonly including employee “snooping” (accessing records of family, friends, coworkers, or celebrities without a work-related need) and other unauthorized disclosures. Risk management objectives focus on preventing these events through role-based access, audit logs with active monitoring, sanctions policies consistently enforced, workforce training, and a culture that treats privacy as patient safety. Even when disclosures are not malicious, “minimum necessary” failures, misdirected faxes/emails, and unsecured devices can create reportable breaches. Effective prevention is layered: technical controls (access restrictions), administrative controls (policies, training), and detection/response (auditing, rapid mitigation). Privacy violations are high-risk because they harm patients, trigger regulatory action, and damage trust and reputation.
According to The Joint Commission, which of the following should be done to patient-owned electrical devices entering the facility?
Options:
inventory with patient belongings
sequester the electrical device
conduct an electrical safety inspection
tag by biomedical engineering
Answer:
CExplanation:
According to Health Care Risk Management standards supported by ASHRM and accreditation guidance from The Joint Commission, patient-owned electrical devices brought into healthcare facilities must be evaluated to ensure they do not pose safety risks. The Joint Commission’s Environment of Care standards emphasize electrical safety, fire prevention, and reduction of hazards within patient care areas.
Before a patient-owned electrical device is used within the facility, an electrical safety inspection should be conducted to assess the integrity of cords, plugs, grounding, and overall condition. The purpose is to identify potential risks such as frayed wiring, overheating hazards, or improper voltage compatibility that could endanger patients, staff, or equipment.
Simply inventorying the device with personal belongings does not address safety concerns. Sequestering the device may be appropriate if it fails inspection, but routine confiscation is not required. While biomedical engineering departments often assist with inspections, tagging by biomedical engineering is not itself the required action; the essential requirement is that a safety inspection be performed.
Clinical and patient safety objectives emphasize proactive hazard identification and compliance with accreditation standards. Therefore, conducting an electrical safety inspection is the appropriate action for patient-owned electrical devices entering the facility.
An employer is not required to offer a reasonable accommodation to a job applicant with a qualified disability unless
Options:
the applicant proves the disability.
withholding the reasonable accommodation creates an unsafe condition.
the applicant requests the accommodation.
the employer recognizes that the accommodation is necessary.
Answer:
CExplanation:
Under Health Care Risk Management principles aligned with ASHRM and the American Hospital Association Certification Center, compliance with the Americans with Disabilities Act ADA requires employers to provide reasonable accommodations to qualified individuals with disabilities. However, the obligation to provide accommodation is generally triggered when the applicant or employee makes the employer aware of the need for accommodation.
The interactive process required by the ADA begins once the applicant requests an accommodation or discloses a need related to a disability. Employers are not required to speculate about potential disabilities or initiate accommodations without notice. While documentation may be requested to verify the disability in certain circumstances, proof is not the triggering requirement. Instead, the request itself initiates the employer’s duty to engage in good faith discussion to determine reasonable accommodation.
Withholding accommodation that creates an unsafe condition may raise separate workplace safety concerns, but that is not the threshold requirement under the ADA. Similarly, an employer’s recognition alone does not automatically impose an obligation absent a request or clear disclosure.
Legal and regulatory objectives emphasize proper documentation, consistent application of ADA standards, and engagement in the interactive process once accommodation is requested. Therefore, the employer’s duty arises when the applicant requests the accommodation.
Which of the following is an essential component of a risk management policy and procedure manual?
Options:
department organizational chart
medical staff bylaws
actuarial report
loss run report
Answer:
AExplanation:
According to Health Care Risk Management standards outlined by ASHRM and the American Hospital Association Certification Center, a risk management policy and procedure manual should clearly define the structure, authority, and operational framework of the risk management program. An organizational chart is an essential component because it identifies reporting relationships, lines of authority, and accountability within the department and in relation to executive leadership and governing bodies.
A clearly documented organizational structure supports regulatory compliance, facilitates communication, and ensures that responsibilities for event reporting, claims management, patient safety initiatives, and regulatory oversight are properly assigned. It also demonstrates governance alignment and helps accrediting bodies evaluate program effectiveness.
Medical staff bylaws are separate governance documents that outline credentialing, peer review, and clinical governance standards. Actuarial reports are financial analyses used in risk financing decisions but are not part of a policy and procedure manual. Loss run reports summarize historical claims activity and support financial review but do not define program structure.
Health Care Operations objectives emphasize formal documentation of authority, processes, and accountability within the risk management framework. Therefore, inclusion of the department organizational chart is an essential element of a comprehensive risk management policy and procedure manual.
A doctor fails to administer an indicated test, and the patient deteriorates and must be admitted. This is an example of:
Options:
Diagnostic error (delay/omission in diagnostic process)
Risk financing error
Contracting breach
Facility security event
Answer:
AExplanation:
Failing to order or perform an indicated test can represent a diagnostic process failure—an omission that delays recognition of deterioration, leading to harm and escalation of care. Risk management objectives treat diagnostic safety as a systems issue: access to decision support, timely follow-up of abnormal results, clear responsibility for test ordering and review, effective handoffs, and adequate staffing/workload conditions to avoid missed steps. Such errors are often linked to underuse in the IOM quality framework (failure to provide beneficial service) and can drive claims due to preventable worsening. Preventive strategies include standardized pathways, trigger tools for abnormal labs, closed-loop test result management, and teamwork practices that encourage escalation when clinical concern persists despite uncertainty.
In enterprise risk management, which of the following are external factors that may affect risk?
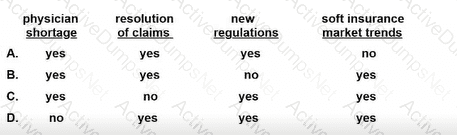
Options:
Option A
Option B
Option C
Option D
Answer:
CExplanation:
According to Health Care Risk Management standards supported by ASHRM and enterprise risk management ERM principles, external factors include conditions outside the direct control of the organization that influence strategic, operational, financial, and regulatory risk exposures.
A physician shortage is an external workforce market condition that can affect staffing stability, access to care, and malpractice exposure. New regulations are also external factors, as legislative or regulatory changes may alter compliance requirements, reimbursement structures, or reporting obligations. Similarly, soft insurance market trends reflect external economic and underwriting environments that influence premium pricing, availability of coverage, and risk financing strategy.
Resolution of claims, however, is generally an internal operational or claims management outcome. While influenced by external legal environments, the resolution process itself is primarily part of internal risk management and litigation strategy rather than a broad external environmental factor.
ERM objectives emphasize analysis of external environmental drivers, including regulatory, workforce, economic, and market conditions. Therefore, physician shortages, new regulations, and soft insurance market trends are external factors affecting risk, while resolution of claims is not primarily classified as external.
An unstable patient in the emergency department needs transfer to another hospital. Which of the following statements is true regarding the refusal of an on-call physician to treat this patient?
Options:
The on-call physician may refuse to participate in the care of any patient, for any reason.
The on-call physician may refuse to participate in the care of a patient, as long as that refusal is not based on insurance status or other financial concerns.
The on-call physician is relieved of duty only if unavailable because of caring for another patient, or because of other circumstances outside the physician's control.
The on-call physician is never relieved of duty to accept a patient needing specialized services.
Answer:
CExplanation:
Under Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, obligations under the Emergency Medical Treatment and Labor Act EMTALA govern on-call physician responsibilities. When a hospital maintains an on-call roster to provide specialty services for emergency department patients, physicians listed on call are required to respond and participate in the evaluation and stabilization of patients with emergency medical conditions.
An on-call physician may only be relieved of duty if legitimately unavailable due to circumstances beyond their control, such as actively caring for another patient or being otherwise unable to respond in accordance with hospital policy. Refusal to treat for convenience or non-clinical reasons may constitute an EMTALA violation and expose both the hospital and physician to regulatory penalties.
A blanket right to refuse care is inconsistent with EMTALA requirements. While financial discrimination is prohibited, refusal for other non-justifiable reasons may still violate federal law. Conversely, stating that a physician is never relieved of duty is inaccurate, as legitimate unavailability may excuse performance under specific circumstances.
Legal and regulatory objectives emphasize compliance with EMTALA, proper on-call coverage policies, and documentation of availability. Therefore, the correct statement is that relief occurs only when the physician is unavailable due to circumstances outside their control.
An organization's chief of orthopedics has scheduled an implant of a new artificial hip for the next day. The chief developed the artificial hip while working as a consultant for a medical device company. The device has not yet been approved by the FDA or the Institutional Review Board. The risk manager's best immediate course of action is to
Options:
contact the FDA to clarify the status of the device.
verify the informed consent for the procedure.
call a special meeting of the Institutional Review Board.
call the chief of surgery to discuss canceling the procedure.
Answer:
DExplanation:
Under Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, the implantation of a medical device that lacks FDA approval and Institutional Review Board oversight presents significant legal and regulatory violations. Use of an unapproved device outside of an approved investigational protocol may violate federal regulations governing human subject research and medical device approval processes.
The risk manager’s primary responsibility is to immediately mitigate regulatory and liability exposure. Because the procedure is scheduled for the next day, urgent intervention is required. Contacting the FDA would not resolve the immediate risk. Verifying informed consent is insufficient, as patient consent cannot legitimize use of an unapproved device outside regulatory pathways. Calling a special IRB meeting would not retroactively authorize an unapproved device without appropriate investigational device exemption processes.
Escalating the issue to the chief of surgery to halt or cancel the procedure is the most appropriate immediate step. This ensures that organizational leadership addresses the compliance violation before patient harm occurs. Risk management objectives emphasize proactive prevention of regulatory breaches, protection of patient safety, and preservation of institutional integrity. Therefore, stopping the procedure is the correct and immediate action.
A hospital risk manager has been called to the Neonatal Intensive Care Unit to discuss a 25-week premature infant whose parents are refusing a planned blood transfusion due to their religious beliefs. After gathering information on the infant’s condition and hearing the parents and the healthcare professionals disagree on the best interests of the infant, the risk manager should
Options:
arrange for an ethics committee consultation to meet the parents and discuss the issue.
prohibit the blood transfusion, respecting the parents’ rights as substitute decision-makers for the infant.
advise the care team to proceed with the blood transfusion.
contact legal counsel to arrange for an emergency court hearing to obtain a court order from the state to intervene.
Answer:
DExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, while parents generally serve as surrogate decision-makers for minors, their authority is not absolute. When refusal of treatment places a child at significant risk of serious harm or death, healthcare providers have an ethical and legal obligation to act in the best interests of the child.
In cases involving life-sustaining treatment for a premature infant, refusal of a medically necessary blood transfusion may constitute potential medical neglect if it threatens the infant’s survival. When disagreement persists after appropriate communication and ethics consultation, and the infant’s life is at risk, the appropriate step is to seek judicial intervention. Contacting legal counsel to obtain an emergency court order allows the state to exercise its parens patriae authority to protect the child’s welfare.
An ethics consultation may help clarify values and promote dialogue but does not override urgent medical necessity. Simply prohibiting or proceeding without legal authority exposes the organization to liability.
Legal and regulatory objectives emphasize protecting vulnerable patients while respecting due process. Therefore, seeking an emergency court order through legal counsel is the appropriate action.
In general, how many steps should an FMEA proceed in each direction (upstream/downstream) when mapping a process for failure analysis?
Options:
Two steps in each direction (a common practical rule-of-thumb)
Ten steps minimum regardless of complexity
Only the current step; context is irrelevant
Steps are not mapped in FMEA
Answer:
AExplanation:
A practical FMEA requires enough process context to capture upstream causes and downstream consequences without becoming unmanageably large. A common operational rule-of-thumb is to examine roughlytwo steps upstream and two steps downstreamfrom a target step to uncover handoffs, dependencies, and failure propagation. Risk management objectives focus on identifying failure modes that originate earlier (e.g., incorrect patient ID at registration leading to lab/specimen mismatch) and harms that emerge later (e.g., delayed result communication causing deterioration). The exact boundary depends on complexity and risk; high-hazard workflows (blood products, surgery, chemo) may require deeper mapping. The goal is usable granularity: map, identify failure modes, score (S–O–D), prioritize, implement controls, and reassess residual risk.
Which of the following should be the primary consideration when designing a new risk management program for a facility?
Options:
size of the facility
type of insurance the facility carries
history of the facility
mission and vision of the facility
Answer:
DExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, the primary consideration in designing a risk management program is alignment with the organization’s mission and vision. A risk management program must support the strategic goals, values, and patient care objectives of the facility. This ensures that risk identification, mitigation strategies, and reporting structures are integrated into the broader organizational framework.
While facility size, insurance structure, and historical claims experience are important operational factors, they are secondary to strategic alignment. The mission and vision guide priorities such as patient safety, quality improvement, regulatory compliance, and financial stewardship. Risk management activities should be structured to advance these priorities, reinforce leadership commitment, and support governance oversight.
An effective program reflects organizational culture, scope of services, and community role. It establishes reporting mechanisms to leadership, integrates enterprise risk management principles, and promotes collaboration across departments.
Health Care Operations objectives emphasize governance integration, strategic alignment, and organizational accountability. Therefore, the mission and vision of the facility should be the primary consideration when designing a new risk management program.
An interrogatory requests insurance policy information. A risk manager should
Options:
provide the specifically requested information.
provide excess limits as well as primary limits.
attach a certificate of insurance.
object to the interrogatory.
Answer:
AExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, insurance policy information is generally discoverable in litigation. Most jurisdictions require disclosure of applicable liability coverage, including policy limits, pursuant to civil procedure rules governing discovery. Therefore, when an interrogatory properly requests insurance policy information, the organization should provide the specifically requested information in coordination with defense counsel.
Providing more information than requested, such as automatically including excess limits if not asked, may exceed the scope of the interrogatory and should be guided by legal counsel. A certificate of insurance is not a substitute for responding to formal discovery requests, as it may not contain all required details regarding coverage, limits, and applicable policy periods.
Objecting to the interrogatory without valid legal grounds is generally inappropriate, as insurance coverage information is typically relevant to potential satisfaction of judgment.
Claims and litigation objectives emphasize cooperation with counsel, compliance with discovery rules, and accurate disclosure of coverage information. Therefore, the appropriate response is to provide the specifically requested insurance policy information in accordance with legal guidance.
Which of the following is the MOST likely root cause of medication errors in healthcare entities?
Options:
manual medication delivery systems
illegible physician handwriting
system or process failure
look-alike, sound-alike drugs
Answer:
CExplanation:
According to Health Care Risk Management standards supported by ASHRM and patient safety principles endorsed by The Joint Commission, the most likely root cause of medication errors is system or process failure. Modern patient safety frameworks emphasize that errors rarely result from isolated individual mistakes. Instead, they typically arise from weaknesses in processes, workflow design, communication systems, technology integration, or inadequate safeguards.
Illegible handwriting, manual systems, and look-alike or sound-alike drugs are recognized contributing factors. However, these elements represent components within a broader system. For example, illegible handwriting becomes problematic when standardized order entry systems are lacking. Look-alike medications pose risks when storage, labeling, or verification processes are insufficient. Manual medication delivery systems increase risk when redundancy and double-check mechanisms are absent.
Root cause analysis methodologies consistently demonstrate that unsafe system design, poor communication processes, lack of standardized procedures, and inadequate training contribute to medication errors. A systems-based approach aligns with just culture principles and focuses on improving processes rather than assigning individual blame.
Clinical and patient safety objectives emphasize system redesign, standardization, and continuous quality improvement. Therefore, system or process failure is the most likely root cause of medication errors.
Which of the following analyses is required as part of the sentinel event process of The Joint Commission?
Options:
fishbone diagram of the causal factors
Pareto chart outlining the problems identified and the priorities for improvement
action plan listing the steps for improvement and the dates of implementation for each step
flow chart listing the responsibilities for each of the departments involved
Answer:
CExplanation:
According to Health Care Risk Management standards supported by ASHRM and the American Hospital Association Certification Center, The Joint Commission’s sentinel event process requires completion of a thorough root cause analysis and development of a corrective action plan. While various analytical tools such as fishbone diagrams, flowcharts, or Pareto charts may be used to assist in identifying contributing factors, these specific tools are not mandated.
The essential required component is a written action plan that identifies specific improvement steps, assigns responsibility, and includes measurable outcomes and timelines for implementation. The action plan must address root causes and system vulnerabilities, not merely individual performance issues. It should demonstrate how corrective actions will reduce the likelihood of recurrence and include monitoring mechanisms to evaluate effectiveness.
Fishbone diagrams and Pareto charts are optional tools used during analysis but are not explicitly required elements. Similarly, departmental flowcharts may support understanding of processes but are not mandated by The Joint Commission.
Clinical and patient safety objectives emphasize systematic investigation, leadership oversight, and documented improvement efforts following sentinel events. Therefore, a detailed action plan with implementation dates is the required analysis component within the sentinel event process.
A sentinel event is a patient safety event that reaches the patient and results in which of the following?
Options:
death, permanent harm, or severe temporary harm
death, temporary harm, or moderate harm
permanent harm, severe temporary harm, or temporary harm
severe temporary harm, moderate harm, or increased length of stay
Answer:
AExplanation:
According to Health Care Risk Management standards supported by ASHRM and The Joint Commission’s sentinel event policy, a sentinel event is defined as a patient safety event that results in death, permanent harm, or severe temporary harm. Severe temporary harm is harm that is critical, life-threatening, or requires major intervention to sustain life, even if the patient ultimately recovers.
Sentinel events signal the need for immediate investigation and response because of the seriousness of the outcome. The Joint Commission requires completion of a root cause analysis and development of an action plan within specified timeframes following awareness of such an event. The focus is on identifying system vulnerabilities and preventing recurrence.
Temporary or moderate harm alone does not meet the sentinel event threshold unless it rises to the level of severe temporary harm. Increased length of stay, without death or significant harm, does not qualify as a sentinel event under the formal definition.
Clinical and patient safety objectives emphasize accurate event classification, structured investigation, and corrective action. Therefore, a sentinel event is one that results in death, permanent harm, or severe temporary harm.
Protecting outdoor air intakes can mitigate the risk of terrorists introducing airborne agents. Steps include:
Options:
Relocate intakes higher; establish a security zone; add lighting and surveillance
Paint the intake vents a different color
Put a “No trespassing” sign only
Reduce HVAC maintenance
Answer:
AExplanation:
Air intake protection is a facility security and safety engineering control to reduce vulnerability to intentional contamination. Elevating intakes reduces easy access; security zones create stand-off distance; lighting and surveillance deter and improve detection. Risk management objectives emphasize layered physical security: access control, environmental design, monitoring, and emergency response planning. In healthcare operations, these measures support resilience and continuity of care, reducing risk of mass exposure events that can overwhelm clinical capacity and cause severe harm.
Which of the following has been proven to reduce costs of workers' compensation programs?
Options:
early return-to-work programs
comprehensive departmental safety analyses
employee assistance programs
employee disciplinary actions
Answer:
AExplanation:
Within Health Care Risk Management frameworks endorsed by ASHRM and the American Hospital Association Certification Center, early return-to-work programs are recognized as one of the most effective strategies for controlling workers' compensation costs. These programs facilitate the safe and timely return of injured employees to modified or transitional duty consistent with medical restrictions.
Workers’ compensation costs are significantly influenced by wage replacement benefits and duration of disability. By reducing the length of time an employee remains off work, early return-to-work initiatives directly decrease indemnity payments, lower claim severity, and improve overall claim outcomes. Additionally, such programs support employee morale, maintain productivity, and reduce the likelihood of prolonged disability or litigation.
While comprehensive safety analyses contribute to injury prevention and long-term risk reduction, their direct cost impact is preventive rather than immediately measurable in claim severity. Employee assistance programs focus primarily on behavioral health and personal support, not claim cost containment. Disciplinary actions do not constitute a structured risk financing strategy and may negatively affect organizational culture.
Therefore, from a risk financing perspective, early return-to-work programs have demonstrated measurable effectiveness in reducing workers' compensation program costs.
For a liability claim to succeed, the claimant must establish duty owed, duty breached, proximate cause, and
Options:
contributory negligence.
injury sustained.
punitive damages.
gross negligence.
Answer:
BExplanation:
Under Health Care Risk Management principles outlined by ASHRM and the American Hospital Association Certification Center, a successful negligence claim requires proof of four essential legal elements: duty, breach of duty, causation, and damages. Duty refers to the legal obligation owed by the healthcare provider to the patient. Breach occurs when the provider fails to meet the applicable standard of care. Proximate cause establishes the direct link between the breach and the harm suffered.
The final required element is actual injury or damages sustained by the claimant. Without demonstrable harm, a negligence claim cannot succeed, even if duty and breach are proven. The injury may include physical harm, emotional distress, or financial loss, but it must be measurable and attributable to the breach.
Contributory negligence is a defense that may reduce or bar recovery but is not an element the claimant must prove. Punitive damages are awarded in exceptional cases involving egregious misconduct and are not required to establish liability. Gross negligence represents a higher degree of negligence but is not a required element in standard malpractice claims.
Therefore, proof of injury sustained is essential for a liability claim to succeed.
A hospital has opted to open an anticoagulation clinic. As this is a high-risk medication, a risk manager wants to conduct a risk assessment before opening the clinic. The BEST tool to use would be a
Options:
root cause analysis RCA.
failure mode and effects analysis FMEA.
cause and effect diagram.
scatter diagram.
Answer:
BExplanation:
Failure Mode and Effects Analysis FMEA is the most appropriate tool in this scenario because it is a proactive risk assessment methodology designed to identify and mitigate potential failures before harm occurs. According to Health Care Risk Management principles outlined by ASHRM and the American Hospital Association Certification Center, FMEA is specifically used when introducing new processes, services, or high-risk clinical operations, such as an anticoagulation clinic involving medications with narrow therapeutic indices and significant bleeding risks.
FMEA systematically evaluates each step in a proposed process, identifies possible failure modes, analyzes their causes and effects, and prioritizes risks using severity, occurrence, and detectability scoring. This structured approach aligns with patient safety objectives by reducing preventable adverse events before implementation.
In contrast, Root Cause Analysis RCA is a retrospective tool used after an adverse event has occurred. A cause and effect diagram is a component often used within RCA or FMEA but is not a comprehensive risk assessment tool on its own. A scatter diagram is primarily used for statistical correlation analysis and does not evaluate process failures.
Therefore, for proactive risk identification and mitigation prior to clinic opening, FMEA is the best and most appropriate tool.
When conducting a safety audit in an Emergency Department, what does an administrator need to obtain first?
Options:
A written set of safety standards/criteria for the audit
A marketing plan
A list of staff birthdays
A patient satisfaction script
Answer:
AExplanation:
A safety audit must be anchored to explicitstandards—policies, regulatory requirements, evidence-based guidelines, and internal procedures—so observations can be evaluated objectively. Without defined criteria, the audit becomes subjective and inconsistent, limiting its usefulness and defensibility. Risk management objectives for ED audits include verifying compliance with high-risk workflows (triage, medication storage, high-alert meds, behavioral health safety, EMTALA processes, handoff communication, alarm management), identifying hazards (environmental risks, crowding, staffing mismatch), and ensuring corrective actions are tracked to closure. A written standard also supports repeatability—audits can be compared over time, and improvements can be measured. This approach aligns with quality management principles: define the requirement, assess the gap, implement controls, and monitor effectiveness.
Which of the following items should be part of a claim file?
peer review reports or data
correspondence with attorneys and investigators
literature search
verification of settlement authority
Options:
1, 2, and 3 only
1, 2, and 4 only
1, 3, and 4 only
2, 3, and 4 only
Answer:
DExplanation:
According to Health Care Risk Management standards outlined by ASHRM and the American Hospital Association Certification Center, claim files must be carefully structured to preserve confidentiality, protect privilege, and support effective defense strategy. A claim file typically includes correspondence with attorneys and investigators, as this documentation reflects legal strategy, communications, and case development. Literature searches relevant to standards of care may also be included to assist counsel in evaluating clinical issues and expert testimony preparation. Verification of settlement authority is essential documentation to confirm that appropriate approvals were obtained before resolving a claim.
Peer review reports or data, however, should not be included in the claim file. Peer review materials are generally protected under state peer review statutes and federal patient safety privilege provisions. Commingling peer review documents within the claims file may jeopardize privilege protections and increase the risk of discoverability in litigation. Maintaining separation between peer review files and claim files is a critical risk management practice.
Claims and litigation objectives emphasize preservation of privilege, organized documentation, and compliance with legal standards. Therefore, correspondence, literature searches, and settlement authority verification belong in the claim file, while peer review reports should be maintained separately.
Unlock CPHRM Features
- CPHRM All Real Exam Questions
- CPHRM Exam easy to use and print PDF format
- Download Free CPHRM Demo (Try before Buy)
- Free Frequent Updates
- 100% Passing Guarantee by Activedumpsnet
Questions & Answers PDF Demo
- CPHRM All Real Exam Questions
- CPHRM Exam easy to use and print PDF format
- Download Free CPHRM Demo (Try before Buy)
- Free Frequent Updates
- 100% Passing Guarantee by Activedumpsnet